“Failing to plan … is … planning to fail.”
(quote attributed to Benjamin Franklin)
On December 13, 1972, Irwin Allen’s arguably most famous disaster flick, The Poseidon Adventure, debuted. Ultimately producing $125 million in box office (that was BIG back then, second only that year to The Godfather), it also produced just one Oscar win, for Best Song, “The Morning After,” immortalized by Maureen McGovern as a single recording released the following year.
The thing about “The Morning After” is that it is a relentlessly optimistic ode to hope – as articulated in the first seven words (“There’s got to be a morning after….”), and that it is perpetually tethered to a movie that resolved a mega-disaster in 117 minutes, with plenty of stars “surviving” the fictional ocean liner capsizing.
At the time we published Part I of this two-part article, no doubt most of your WSR editors believed, or at least fondly wished, that we’d see a similarly time-scaled result with the coronavirus pandemic. At this writing, hope for such a quick resolution is in short supply.
[Ed Note: To put this article in the context of the ever-evolving health crisis, at the time of this writing the USA had just announced the largest quarterly decline in GDP in our nation’s history (-32.9%), the death toll had exceeded 160,000, state and local governments were facing massive budget cuts, major league sports of various kinds were struggling to re-open in abbreviated seasons, there had been a cumulative 58 million initial unemployment filings since March 1 and the latest announced monthly unemployment rate exceeded 10%, parents nationwide were trying to decide how and when to send their children back to school, and Congress and the White House were arguing over the terms of the next COVID rescue package.]
Creating a Safer Workplace
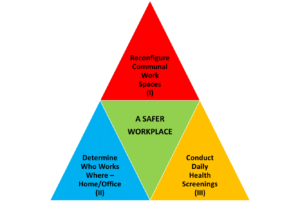
Fig. 1: Three Required Processes for a Safer Workplace in the Age of COVID
Figure 1 illustrates the three required elements of the safer workplace for which all employers must strive in the age of the coronavirus. Phase I, which should be complete before reopening, involves redesigning communal work spaces to reduce congestion, increase social distancing, and perhaps even improve or modernize air circulation systems. While this subject is not related to human capital management and therefore beyond the scope of this article, the web is full of great articles on the topic (see, e.g., Fast Company’s excellent April 30, 2020, article covering open office redesign1.)
Phase II, which will be discussed below, is the determination of which employees will work from home and which will return to communal office space. While the EEOC and CDC offer employers some guiding principles in this regard, there are no hard-and-fast rules, and HR professionals may find this to be a time-consuming process requiring highly detailed recordkeeping. This phase can be mostly completed prior to reopening, but will continue indefinitely, given there will be new hires and changes in worker circumstances over time.
Phase III, which for most employers will continue at least until an effective vaccine has been made available and statistics local to each office space reflect minimal viral transmission, involves performing daily health checks for each employee on entrance to the communal space. This will also be discussed in detail below.
Let’s Stop Calling It “The New Normal”
One thing this pandemic has proven NOT to be is predictable! So far, the pandemic has been moving through a series of phases which can only be called “temporary abnormals.” So how do we best prepare for the near-term abnormal: re-opening workplaces in a constantly shifting environment of fear and uncertainty?
In crises gone by (9/11, economic downturns such as the 2008 recession), employers could expect various federal regulations to spin off, instructing them precisely what steps they had to take to remain in compliance and avoid exacerbation or repeat of the circumstances that caused the problems. And the FFCRA and CARES Act (discussed in detail in the last issue of WSR) started out leading employers to believe that this crisis would be treated the same way. But as April began, employers wondered what specific re-opening rules and regulations would be issued by regulatory bodies such as OSHA, the CDC, HHS, or the Department of Labor. As of this writing, employers are still waiting.
The CDC Weighs In
On May 14, the Centers for Disease Control issued a set of six re-opening guidelines for key societal components such as workplaces, schools and childcare operations, restaurants and bars, camps, and mass transit operations. The workplace instructions looked like this:
Fig. 2: CDC Workplace Re-Opening Guidelines – issued May 14, 2020
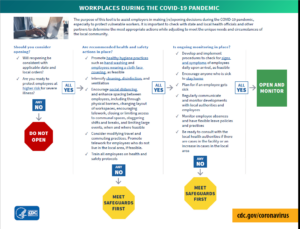
It should be noted that this infographic has since been deleted from the CDC’s website and replaced with narrative, last updated May 6, and located here2 . What is most striking about both the flow-chart above, and the narrative which replaced it, is the stark absence of any form of mandate within the guidance. Every step is worded in the “advisory voice” rather than the “mandatory voice.” Many steps end with phrases like “as feasible,” “if feasible,” “where feasible,” or “if possible.” Compare this style with how covered employers are advised by the same federal government to comply with FMLA, EEO/AAP, OSHA, ACA or HIPAA. These previous regulations all carry substantial monetary penalties for violations, some also include the threat of civil litigation, and the last (HIPAA) even references criminal penalties for certain intentional violations! Given this lack of explicit regulation, how exactly does an employer re-open a communal workplace safely? In other words, where are the “rules”?
The Basic Mandate: OSHA Compliance
Given the lack of specific mandates within the May CDC guidelines, it would be fair to begin by asking whether there is even a basis for mandating that employers do anything affirmatively to protect employees from coronavirus infection, beyond keeping a reasonably clean workplace. The answer to this question can be found in the Occupational Safety and Health Act of 1970 (“OSH”), and two specific doctrines emanating from it: the general duty clause, and the imminent danger clause.
The general duty clause of the OSH Act specifies, in pertinent part, that employers must provide each worker “employment and a place of employment, which are free from recognized hazards that are causing or are likely to cause death or serious physical harm.” Given recent statements from the CDC about COVID-19, and the infection and death rate in this country, it is virtually indisputable that the coronavirus would qualify as a “recognized hazard” under the OSH Act. Consistent with that view, in March of 2020, the EEOC issued guidance3 that the COVID-19 pandemic does meet their definition of a “direct threat” to employees or others with whom the employee may come into contact.
Much as the general duty clause imposes an obligation on employers, the imminent danger clause offers employees a qualified right to opt-out of continuing to work or returning to work in an inherently dangerous environment. The clause allows employees to refuse to work if they believe they are in “imminent danger” because death or serious injury could result from working in the dangerous environment. As of this writing, no court has yet ruled that an employee can refuse to report to work simply because of a generalized fear of contracting COVID-19, even if that employee is at heightened risk due to age or comorbidities, and OSHA has been silent on the subject.
In fact, the only experience that the employer community has so far on the applicability of the imminent danger doctrine to the pandemic, occurred when the President signed an Executive Order (EO 139174) on April 28, invoking the Defense Production Act to “ensure that Americans have a reliable supply of [food] products…” The Order was immediately challenged in court, with the plaintiff workers alliance contending that they were being ordered back to work, shoulder to shoulder, with insufficient PPE or protective barriers to avoid transmission of viral infection. The federal district court ruled for the defendant food processor plant employers and dismissed the suit on May 5, on the basis that OSHA had jurisdiction and must be given time to issue further guidelines [Rural Community Worker’s Alliance et al v. Smithfield Foods, Inc. et al5]. As of this writing, those “further OSHA guidelines” have yet to be issued.
The Most Important Decision: Who Works Where?
Despite the lack of general OSHA guidance – let alone specific regulations – on re-opening communal workspaces, employers have no choice but to address the process. This includes a multiplicity of decisions to make – about workspace re-design and ergonomics, about workforce management (“shift-shifting” to reduce the number of workers in a space at any given time), and perhaps most importantly, about which employees continue to work from home and who comes in to the office – and how often?
While the “imminent danger” doctrine of the OSH Act (so far) does not apply, the Americans with Disabilities Act still does, and it may be necessary for employers to make certain accommodations for employees returning to communal work locations. For these employer decisions, the EEOC, which is the enforcement agency behind the ADA, has issued guidelines, and they can be quite useful for employers6. For example:
- The EEOC guidelines permit the employer to request of an employee specific details about the reasons for their accommodation request.
- In the case of a work-from-home request, these details might include some combination of the employee’s age (presumably already known to the employer) and recognized COVID comorbidities that make them more sensitive to a serious or even fatal outcome. Note that while these inquiries were previously not permitted for “regular” (e.g., seasonal influenza) pandemics, the nature of the COVID crisis has changed these rules7.
- While employers may adopt reasonable infection control standards and require employees to comply with them, e.g., frequent hand washing, cough/sneeze etiquette, wearing of PPE and face masks; employers may not compel their employees to accept any future vaccine developed to fight COVID (e.g., over the medical or religious objections of those employees.)
- These guidelines should be considered mandatory reading, because they go on to answer several important questions which would likely come up for almost every employer. Two examples of likely universal interest:
-
- (Q.D138) Question: Must an employer consider an employee’s requested accommodation (e.g., to work from home), not because of the employee’s own advanced age and/or comorbidity, but rather the fact that their grandparents live in their household and they fear picking up the virus “silently” and bringing it home? Answer: No. The ADA protects the employee – not other members of the employee’s household.
- (Q.C49) Question: May an employer withdraw a job offer where the individual is needed to start immediately but the applicant has COVID-19 or its symptoms? Answer: Yes. Since the individual cannot enter the workplace safely and the job fill need is immediate, the offer may be withdrawn.
In addition to staying current on updates published by the EEOC, the Centers for Disease Control should inform employers’ decisions about “who works where”. Since the early days of the pandemic, the CDC has been the definitive authority on comorbidities (pre-existing conditions) which can turn a case of COVID-19 from an inconvenient bad case of the flu into a life-threatening disease. But on June 25, 2020, the CDC greatly expanded that list of comorbidities. See Fig. 3 for a summary of those changes, and note that the most recent changes to the list are highlighted in red:
Fig. 3: CDC Revised List of COVID Comorbidities (Updated June 25, 2020)10
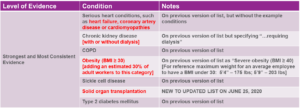
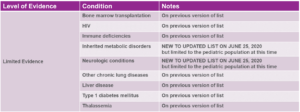
Several days before the CDC announced these revisions, Kaiser Family Foundation published a finding that “Almost One in Four Adult Workers is Vulnerable to Severe Illness from COVID-19”.11 In this article, KFF enumerated that as of 2018 (the latest statistics available), there are 10 million working adults who are age 65 or over, and an additional 27.7 million working adults under age 65 who are at heightened risk due to reported comorbidities.
With the CDC’s June additions to the above list, particularly the reduction of the “danger level” of body mass index (height-to-weight ratio) from 40 to 30, the proportion of at-risk adult workers could easily increase from 24% to more than 50% nationwide.
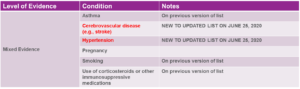
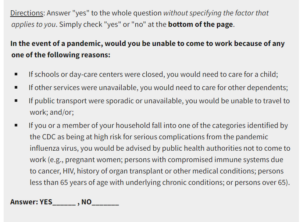
Finally, employers must bear in mind the EEOC ADA guidelines for inquiring about comorbidities and symptomology. The guidelines require that the employer structure their inquiry so that the employee gives one answer of “yes” or “no” to the whole question without identifying the specific factors that apply to him/her. Fig. 4 is an example of an EEOC-compliant questionnaire. Although offered as a “pre-pandemic employee survey,” a version of this inquiry could be used mid-pandemic for employers planning which employees return to the communal workspace, and be modified to include the latest “strongest and most convincing evidence” conditions listed by the CDC (in Fig. 3, above) :
Fig. 4: ADA-Compliant Pre-Pandemic Employee Planning Survey12
Accessing the Workplace: Daily Health Checks
Once the decision is made as to who will come into an employer’s communal workspace and on what frequency, and any redesign principles have been leveraged to make the workplace as safe as possible, the third leg of the “COVID transmission prevention pyramid” (see Fig. 1) involves designing and administering a health check regimen for employees. Most employers will want this process to be executed on each employee’s arrival to work, each day, and some states require it.
As previously discussed, due to the unprecedented severity of the COVID pandemic, the EEOC has granted employers broad exceptions to permit the taking of employees’ temperatures, and assessment of symptoms via a question-and-answer exam.
While some employers may make the decision to have the process of temperature measurement and symptom assessment handled by healthcare or HR professional staff, others may find this to be impractical – for example, if they are using staggered starting and end times to reduce employee concentration over, say, a 12-hour day. For employers not wanting to dedicate one or more staff members over the course of each day for check-ins, there are technology alternatives available.
Multiple vendors offer thermometric devices that integrate directly into either timeclocks, facility access devices, or both. The best timeclock enhancements for COVID screening not only allow for quick, non-contact temperature assessment, but also interactive symptom checking, and even voice-activated (touch-free) operation. (Fig. 5)
Fig. 5: Staffing-Free Temperature Checking (Timeclock Integration)
The EEOC, charged with enforcing ADA rules, issued a special advisory as early as March of this year (and updated since), specifically authorizing employers to not only take employee temperatures, but to question employees about COVID symptoms13. Best practice, aligned with EEOC/ADA guidance14, would require that:
- The temperature be taken from a safe distance by the least invasive means possible (e.g., infrared or thermal scan),
- All questions be clearly related to published COVID symptomatology,
- Some degree of privacy is afforded to employees as they answer them,
- The employee be referred to an HR, Risk Management or onsite healthcare professional by the clock or entry device if answers require further follow-up or the employee reflects an unacceptable level of body fever, and
- The results of each exam must be treated with the confidentiality that ADA records in general require.
HCM Implications: There has been a fair amount of misunderstanding about whether taking temperatures and asking questions on a routine basis constitutes a “medical examination” under the ADA or the Occupational Safety & Health Act of 1970, and therefore triggers both higher confidentiality requirements, and a record retention rule of “employee’s length of employment plus 30 years.” The EEOC has clarified, in their COVID-specific guidance15 that, provided the examination is NOT being conducted by a healthcare professional, no such higher scrutiny attaches to the record made by the access point system. This is another potential argument for using timeclocks or point of access devices, rather than trained healthcare professionals, for routine daily health checks.
Business Travel Just Got More Complicated
Many years ago, HR professionals might have had to keep records of foreign travel when employees traveled internationally to disease-impacted nations or areas of significant political upheaval. In the “near-term abnormal,” some employers may find it necessary to keep a historical record of domestic business travel to address the possibility of a mandatory quarantine period imposed on a traveler, or when a COVID “hot-spot” is identified, as they so often are, after the fact.
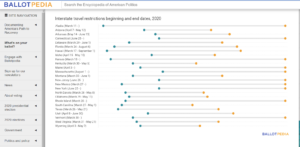
There are multiple sources available to HCM professionals to track this ever-changing set of restrictions. The CDC has published an excellent overall guide to travel safety16, which it keeps updated for the latest developments. And Ballotpedia keeps an updated detail on all 50 states’ travel restrictions, both current and historical17. See Fig. 6 for the current historical snapshot as this article was being written.
The bottom line: before that Vice-President boards the plane to visit the office in [fill in name of state here], it would be important to know whether she will be subject to a self-quarantine period on arrival. Further, if a business traveler returns from [fill in name of city here], and that night on the news it’s reported that there has been a major coronavirus outbreak there, it could be important to have a record of the state, city, specific location, and perhaps even the hotel/lodging where that employee stayed.
Fig. 6: Ballotpedia: Interstate Travel Restrictions Beginning and End Dates, 2020
The State of Virginia Would Like a Brief Word…
In 1607, Virginia was the first area to be settled by the English in the New World, and 413 years later, they became the first state to impose statewide restrictions on employers reopening workplaces during the “near-term abnormal.” Specifically citing the lack of guidance from OSHA, on July 15, 2020, Virginia Governor Ralph Northam published, effective July 27, 2020, a set of regulations applicable to any employer operating a work location within state borders18.
The statewide emergency safety standards adopted by Virginia are temporary, for six months, but renewable after that. They require, among other things, classification of the risk of exposure for all jobs as either very high, high, medium or lower, prescreening or surveying of employees for COVID symptoms prior to each work shift, and the prevention of employees demonstrating symptoms of the disease from accessing the work place19. The new workplace safety standards also include multiple employee training and re-training requirements, but those provisions have had their effective dates delayed to August 26 or September 25, 202020.
While Virginia was first to publish and begin enforcing new COVID safety guidelines, it is clear that other states are anxiously observing Virginia’s experience for possible guidelines of their own. And many states already have specific guidelines related solely to employee temperature assessment and/or symptom survey administration. The Littler law firm publishes, and keeps updated daily, a survey of all 50 states laws around temperatures and symptom surveys, which can be essential reading for multi-state employers21.
Moving Forward From Here
This pandemic has resisted all attempts to predict its course. The most expert professionals cannot tell us where we are in the overall course of the disease, and as a result HCM professionals must remain flexible and responsive to their HR customers to provide the information they need to make informed decisions.
[Ed. Note: As this article was nearing completion, the President had just signed several coronavirus-related Executive Orders and Presidential Memoranda. One of these memos confers a never-before-seen “Payroll Tax Holiday” on the American people which, if it withstands judicial challenge, could require a significant redesign of the tax calculation and remittance routines of virtually every payroll system in the country. Stay tuned!]
Endnotes:
1 https://www.fastcompany.com/90498002/from-officles-to-giant-sneeze-guards-how-covid-19-will-change-your-open-office
2 https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-business-response.html
3 https://www.eeoc.gov/sites/default/files/2020-04/pandemic_flu.pdf
4 https://www.whitehouse.gov/briefings-statements/president-donald-j-trump-taking-action-ensure-safety-nations-food-supply-chain/
5 https://www.govinfo.gov/app/details/USCOURTS-mowd-5_20-cv-06063/summary
6 https://www.eeoc.gov/wysk/what-you-should-know-about-covid-19-and-ada-rehabilitation-act-and-other-eeo-laws
7 “Asking employees if they are immuno-compromised or have a chronic condition is a disability-related inquiry subject to the ADA’s restrictions. When pandemic influenza symptoms only resemble those of seasonal influenza, they do not provide an objective basis for a “reasonable belief” that employees will face a direct threat if they become ill. Therefore, they do not justify disability-related inquiries or medical examinations.”, …however…
“If an influenza pandemic becomes more severe or serious according to the assessment of local, state or federal public health officials, ADA-covered employers may have sufficient objective information from public health advisories to reasonably conclude that employees will face a direct threat if they contract pandemic influenza. Only in this circumstance may ADA-covered employers make disability-related inquiries or require medical examinations of asymptomatic employees to identify those at higher risk of influenza complications.” [emphasis added]. https://www.eeoc.gov/laws/guidance/pandemic-preparedness-workplace-and-americans-disabilities-act#34
8 https://www.eeoc.gov/wysk/what-you-should-know-about-covid-19-and-ada-rehabilitation-act-and-other-eeo-laws
9 Ibid.
10 https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html
11 https://www.kff.org/coronavirus-covid-19/issue-brief/almost-one-in-four-adult-workers-is-vulnerable-to-severe-illness-from-covid-19/
12 https://www.eeoc.gov/laws/guidance/pandemic-preparedness-workplace-and-americans-disabilities-act#34
13 https://www.eeoc.gov/wysk/what-you-should-know-about-covid-19-and-ada-rehabilitation-act-and-other-eeo-laws
14 https://www.eeoc.gov/laws/guidance/pandemic-preparedness-workplace-and-americans-disabilities-act#34
15 Ibid.
16 https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html
17 https://ballotpedia.org/Travel_restrictions_issued_by_states_in_response_to_the_coronavirus_(COVID-19)_pandemic,_2020#Map_of_active_travel_restrictions_by_state
18 https://www.governor.virginia.gov/newsroom/all-releases/2020/july/headline-859234-en.html
19 https://www.doli.virginia.gov/wp-content/uploads/2020/07/RIS-filed-RTD-Final-ETS-7.24.2020.pdf
20 Ibid.
21 https://www.littler.com/publication-press/publication/wont-hurt-bit-employee-temperature-and-health-screenings-list



